An enduring affiliation
Pauley physicians provide cardiovascular care to veterans at the VA
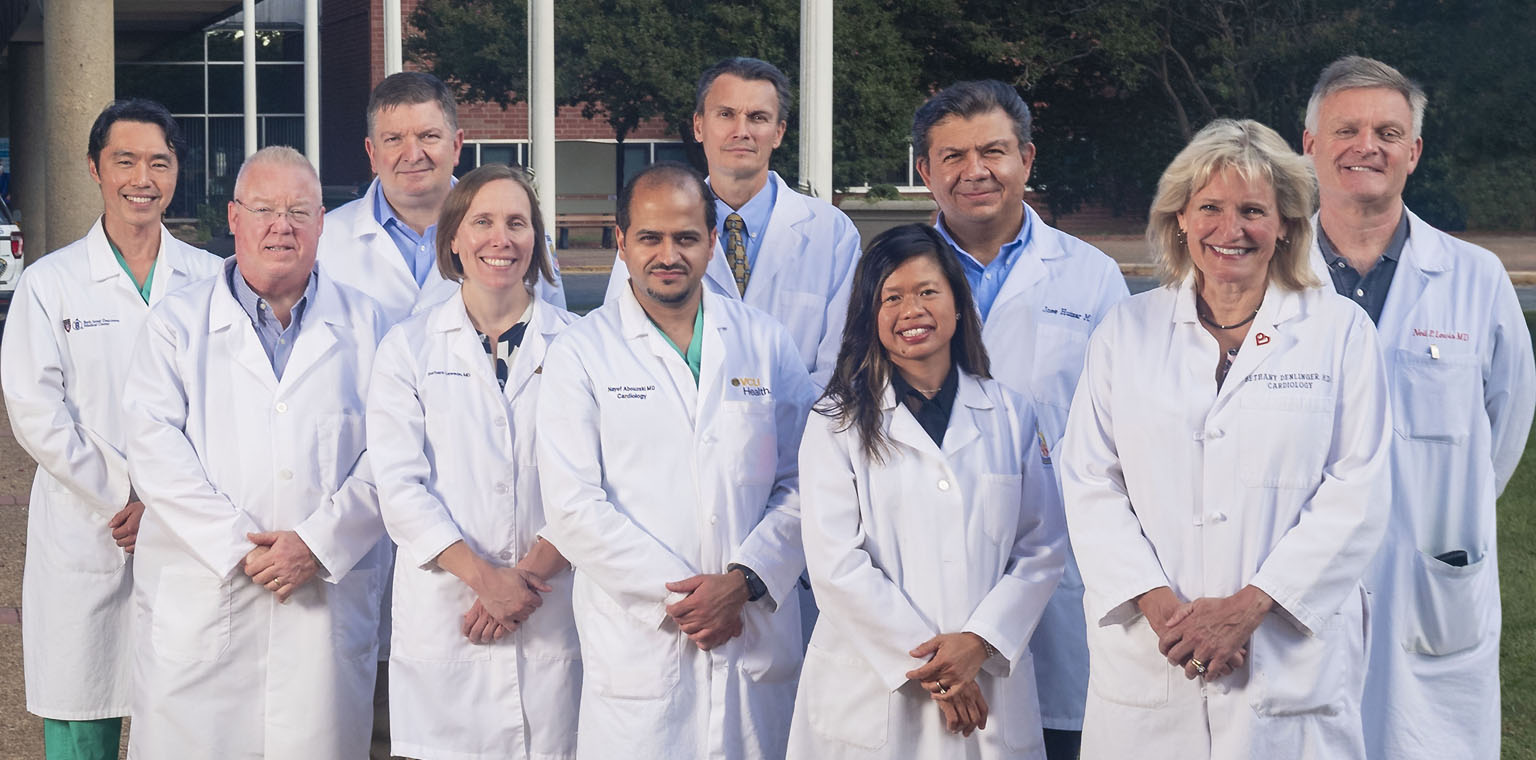
Front row (L to R): John Boyle, Barbara Lawson, M.D., Nayef Abouzaki, M.D., Lea Lander, Bethany Denlinger, M.D. Back row (L to R): Alex Tan, M.D., Ion Jovin, M.D., Karoly Kaszala, M.D., Jose Huizar, M.D., Neil Lewis, M.D.
Millions of Americans suffer from cardiovascular disease, and the risk of developing it may be even higher for our nation’s veterans. The Department of Veterans Affairs reports that cardiovascular disease is the leading cause of death among veterans enrolled in the VA health care system.

Cardiovascular services available to veterans at CVHCS in Richmond run the gamut from noninvasive diagnostic tests to surgeries including heart transplants. In addition to clinical care, the affiliation includes teaching and research activities, with many staff physicians having faculty appointments at VCU Medical Center.
“I’ve worked for the VA full or part time since 1990,” Lesnefsky said. “What attracted me were the academic opportunities and the research opportunities. What’s kept me here are the service opportunities and the ability to provide care to a very appreciative patient population.”
Dr. Karoly Kaszala and EP team perform a procedure in the VA electrophysiology lab. Other team members pictured are Dr. Ajay Pillai, electrophysiology fellow at the operating table, Dr. Darrin Gould from anesthesiology and nurse Nathalie Tomety assisting at the recording system.
Clinical excellence
CVHCS in Richmond has a strong track record in cardiac surgery and cardiac transplantation. In 1980, it became the first hospital in the VA system to conduct heart transplant surgery. The transplant program thrived for decades under the vision and expertise of cardiothoracic surgeon Szabolcs Szentpetery, M.D.Several physicians who became leaders in the field of cardiology at VCU Health started their careers at CVHCS in Richmond. Szentpetery mentored Vigneshwar Kasirajan, M.D., the Stuart McGuire Professor and Chair of the Department of Surgery at VCU Medical Center, and Kenneth Ellenbogen, M.D., the Martha M. and Harold W. Kimmerling Chair of Cardiology, VCU School of Medicine, and director of clinical cardiac electrophysiology and pacing at VCU Medical Center.
Today, under the direction of medical director Neil Lewis, M.D., the Heart Failure/Transplant Program continues to be on the cutting edge of transplant medicine. For example, CVHCS in Richmond was the first VA medical center in the country to offer a Left Ventricular Assist Device (LVAD) as a bridge to transplant and has implanted more than 200 LVADs since 1992. “This technology has allowed us to provide the sickest patients the opportunity to improve their overall state of health, thereby increasing the opportunity for a successful outcome following transplantation,” Lesnefsky said.
CVHCS in Richmond is a member of the VA Mid-Atlantic Health Care Network, one of the VA’s 18 regional networks of hospitals in the Veterans Integrated Services Network (VISN). The Richmond site, in VISN 6, works closely with centers in Hampton, southwestern Virginia and western North Carolina to provide and improve access to cardiovascular services. Patients are referred to CVHCS in Richmond from across the mid-Atlantic. “We truly have not only regional reach, but reach beyond that,” Lesnefsky said.
CVHCS in Richmond employs full-time and part-time Pauley-affiliated cardiologists with years of expertise in the areas of advanced heart failure and heart transplant, electrophysiology, interventional cardiology and noninvasive cardiology. “We perform most procedures that are available at any university hospital,” Lesnefsky said. What’s more, CVHCS is the only VA hospital in the country to perform heart transplants on site.
“I want the community to know that we provide world-class care at the Central Virginia VA Health Care System,” said Nayef Abouzaki, M.D., an interventional cardiologist and site director at CVHCS for the VCUHS cardiology fellowship. “Our goal is to provide our veterans with the best outcomes by decreasing the morbidity and mortality of very advanced cardiovascular conditions — whether that’s peripheral arterial disease, where we’re preventing amputations; whether that’s significant coronary artery disease, that we can refer patients for bypass surgeries or do complex cases to regain blood flow and recover the heart; or whether that’s patients with advanced heart failure who need LVAD devices to support their heart, or even heart transplant. All of this is done in partnership with the Pauley Heart Center.”
Working with veterans can be profoundly moving and memorable. Abouzaki recalled helping a veteran who’d had a heart attack get back to doing what he loved: preaching to inmates at a correctional facility. Not a good candidate for heart surgery, the patient languished at home for weeks, sleeping in a chair and feeling dispirited. Abouzaki intervened and suggested stents to optimize blood flow to the heart. The procedure was high risk but successful.
Eight stents and two years later, the patient is doing well. His heart recovered. “He’s sleeping back in his own bed, not in the recliner, and is back to preaching again,” Abouzaki said. “He’s very appreciative. It was the most rewarding, gratifying experience for me.”
Complex cases and grateful patients keep Abouzaki and his colleagues energized.
“I’m proud of being at the VA,” Abouzaki added. “It’s really a privilege for me to work at the VA and to be part of the Pauley Heart Center as well.”
“It is an honor to give back to those who have served our country,” said Bethany Denlinger, M.D., medical director of the echocardiography lab and cardiac rehab at VCU Health Community Memorial Hospital in South Hill, Virginia. She splits her time between South Hill and Richmond, where she works two days a week in the echo lab at CVHCS.
Jonah Pozen, M.D., VCU Health Pauley Heart Center assistant professor of medicine and Central Virginia VA Health Care System staff cardiologist, speaks with fellows Kunal Kapoor, M.D., Anna Tomdio, M.D., and Pengyang Li, M.D., as they review patients in the VA Cardiology subspeciality clinic.
Research excellence
The VA is a significant source of funding for cardiovascular disease research. Its Merit Review Award program supports investigator-initiated research focused on veterans’ needs and allows investigators to collaborate with academic institutions. Merit Review Award grants are highly competitive and on par with those offered by the National Institutes of Health. More than 60% of VA researchers are also clinicians who provide direct patient care.Merit Review grant recipients at CVHCS in Richmond’s division of cardiology and their respective areas of research include Lesnefsky (metabolic mechanisms of cardiac dysfunction with aging), electrophysiologist Jose Huizar, M.D. (premature ventricular contraction-induced cardiomyopathy) and electrophysiologist Alex Tan, M.D. (cardiac arrhythmias and cardiac neuro function). A Merit Review grant is also supporting cardiac surgeon Mohammed Quader, M.D., as he studies how to metabolically rehabilitate hearts after circulatory death, an investigation that could one day help further expand the number of hearts suitable for transplantation.
The VA also has a research grant program for nonclinician (Ph.D.) investigators to help expand its portfolio of science relative to cardiovascular disease. Pauley-affiliated investigator Ashley Cowart, Ph.D., a professor in the Department of Biochemistry and Molecular Biology in the VCU School of Medicine, is studying a specific class of lipids known as sphingolipids and the role that they play in obesity-related diseases such as diabetes. Veterans suffer from these diseases at a disproportionate rate relative to the general population and are strongly linked with post-traumatic stress disorder, which is considered predictive of diabetes, she said. Shobha Ghosh, Ph.D., a professor of medicine and physiology at the VCU School of Medicine, is funded to study the mechanisms of atherosclerosis.
Huizar, director of the Arrhythmia and Device Clinic at CVHCS in Richmond, provides patients with ablative therapies while leading research into PVC-induced cardiomyopathy. A research-dedicated 1.5 Tesla MRI scanner requested by Huizar and supported by a VA grant will arrive by 2023 and will be used by physician scientists across several fields to expand their research. The 1.5T-MRI also will open new opportunities for multiple investigators to participate and collaborate in national and international research studies.
The VA has been a leader in multisite, randomized-control clinical trials going back five decades to the first randomized-control trial that showed coronary artery bypass grafting surgery works to improve survival in patients with a specific high-risk heart artery blockage. A soon-to-be-recruiting randomized clinical trial called RICH (remote ischemic preconditioning for renal and cardiac protection in congestive heart failure) will examine ischemic preconditioning in patients with heart failure, “something researchers have looked at mostly in the setting of myocardial infarction and stroke,” said Ion Jovin, M.D., director of the Cardiac Catheterization Laboratory and deputy chief of cardiology at CVHCS in Richmond.
A frequent multisite trial participant, Jovin is co-investigator with the VA Pittsburgh Healthcare System for RICH. “Ischemic preconditioning aims to protect the heart muscle or the brain from the damage that occurs during a myocardial infarction or a stroke, but the mechanisms of this protection are not well understood,” he said.
Education excellence
Cardiology and interventional cardiology fellows at VCU Medical Center have a required rotation through CVHCS in Richmond. The VA funds a number of those positions, which provide early-career physicians significant cath lab, invasive cardiology and interventional cardiology training. “We have fellows in clinics, in the inpatient services, triaging patients from the emergency room and admitting them to the ICU or to the general ward to stabilize their heart condition,” said Abouzaki, who trained in the CVHCS cath lab in both coronary and leg artery interventions for patients at risk of amputation. “We have fellows on imaging rotations. We have them in the cath lab. They’re present 365 days.”The veterans appreciate the fellows’ attentive care, Abouzaki said, and the fellows appreciate the veterans’ dogged determination. “They’re tough patients. They want to live longer, and they fight and fight — all the way to the end.”
What’s next
Barbara Lawson, M.D., a specialist in interventional and structural cardiology, is building the much anticipated transcatheter aortic valve replacement (TAVR) program. “For the past five years, I have brought the veterans to VCU for TAVR procedures performed by myself and Dr. Mohammed Quader,” she said. “Building a program at the VA will obviate the need to transition care between centers, streamlining the referral process and expediting their care.”
On the educational side, Lesnefsky envisions “continuing to improve the experience for our fellows by providing opportunities for them to demonstrate initiative and clinical ownership.”
These measures, and more, will ensure that those who served our country in the armed services have — and continue to have — the best possible chance at a long and healthy life.




