A New Chapter Begins
Learn how cardiovascular care is evolving at Pauley with a new director and mission.
Our world-class team takes your heart health personally.
Building on our history of innovation in patient care, scientific discovery, diversity and collaboration, we improve cardiovascular care for all, while continuously training the next generation of doctors.
These words articulate a new mission, recently unveiled by Pauley. “The new mission reflects the changing terrain of cardiovascular care,” said Director Dr. Greg Hundley.
This changing terrain takes many forms. For instance, while Pauley was once limited to downtown, its reach now extends to communities such as South Hill, Colonial Heights and Williamsburg through outreach clinics and hospitals.
“The expansion of our footprint is critical to bringing Pauley’s exceptional cardiovascular care to all who need it in our state,” said Hundley.
The mission also speaks to the terrains of patient care, scientific discovery and training the next generation of doctors—and the direction Pauley must turn to continue its long history of innovation in these areas.
“In recent years, there has been enormous growth within cardiovascular medicine and cardiovascular surgery,” he said. “At the same time, exciting opportunities have arisen through new partnerships with partners in Oncology, Pharmacy, Pharmacology and Physiology, Behavioral Science, Kinesiology and Exercise, Biomedical Engineering, Population Health and issues related to societal demographics.”
To encompass both the growth within the traditional fields and expand beyond, he said, the heart center needed to come together to develop a new mission to carry it forward for the next 20 years.
“Collaboration will be one of the keys to attaining our mission, and it’s already taking place every day at Pauley,” he said.
It’s 7:30 a.m., and physiologist Dr. Justin Canada is overseeing an innovative MRI procedure in the Cardiovascular Imaging Suite in the North Hospital. The room is full of monitors, which Canada and the other members of his team continually check. One screen shows the black and white image of a patient’s beating heart.
“Please breathe in, breathe out. Now, hold your breath.”
On the other side of a glass wall from them, the patient, lying inside an open-sided magnetic resonance imaging (MRI), follows the directions. There’s a long beep as her chest scan begins. She is the first patient in this pilot study. During the scan, she pedals a supine exercise bike attached to her table. The harder she pedals, the more her heart rate and VO2 levels—the volume of oxygen that her body uses for metabolic work—spike up.
This is a new diagnostic tool. VCU Medical Center is one of only a handful of centers in the world where this is possible: real-time MRI imaging during an exercise stress test.
“The expansion of our footprint is critical to bringing Pauley’s exceptional cardiovascular care to all who need it in our state,” said Hundley.
“It’s very exciting—I’m stoked,” said Canada, principal investigator for the study.
He is measuring the cardiorespiratory fitness of cancer patients who are undergoing evaluation for bone marrow transplantations, then comparing the results to that of age- and gender-matched healthy individuals, like this morning’s patient. Through the study, he hopes to establish a protocol for determining the specific causes of exercise intolerance in those with cancer, which may have future applications in the assessment of cardiotoxicity in cancer survivors.
“Cancer-related fatigue is the most predominant quality-of-life disabling symptom of the cancer patient,” he said. “With this technique, we’ll be able to look at how much a person’s exercise capacity is related to the heart’s capacity to pump blood and/or the muscles’ ability to extract oxygen. The advantage is, this can be done noninvasively, without the need for measures such as cardiac catheterization or exposure to radiation.”
Co-Investigator Dr. Jennifer Jordan, a biomedical engineer who directs the lab, watches the screens to see if any adjustments are needed for the scans. She’s there to determine “the best way to acquire those images and optimize the protocol—both to get good, crisp pictures and also to reduce patient burden,” she said. “We don’t want someone in the scanner exercising for 60 minutes when we can get them in and out in 15 minutes.”
MRI sessions can involve a series of 1,000 photographs that in many facilities can take 45 minutes to an hour to complete. Pauley’s Siemens Magnetom Vida 3T MRI system can complete similar sessions in 15 minutes. In addition to speed, the system offers extraordinary resolution.
Jordan took part in a similar study at another facility, where the team had to move patients back and forth between a treadmill and a scanner. “Each time, there was a 20-second delay. During that time, the heart rate was already starting to recover. But with the scanner we have here, and the supine bike, Dr. Canada is going to be able to answer that question of: What does that peak heart function really look like?”
The mission control atmosphere in the room, and the makeup of the medical team, also reflects a new approach to cardiology.
“We’ve got an engineer, a cardiologist, an exercise physiologist and an MRI technician. This is a team from across multiple disciplines, across both VCU campuses,” said Hundley, who is observing the study. “We are assembling to address our challenges. And that’s needed because the disease processes that we are managing today are complicated.”
In the clinical setting, multidisciplinary teams are playing a key role in tackling tough situations. For instance, Pauley’s Coronary Intensive Care Unit (CICU) is taking part in a joint program with the Obstetrics and Labor and Delivery Departments that involves early identification of high-risk maternity patients with cardiovascular disease. Patients with existing cardiovascular conditions are especially vulnerable during pregnancy, which can place a significant burden on the heart.
“By the third trimester, you can increase your cardiac output almost 50% during pregnancy and your blood volume expands 30-40% higher than normal. That increase in fluid can also put stress on the heart,” said Jennifer Powers, one of the CICU nursing leaders of the Complex Maternal Cardiac Care Group along with Kerry Patterson and Charlotte Roberts.
The pilot program started five years ago and focused on maternity patients who have advanced heart failure, coronary heart disease with prior heart attacks and congenital heart disease—all of which have been on the uptick in recent years in this population. One troubling condition is hypertrophic cardiomyopathy, which causes an abnormal thickening of the heart muscle that can affect the heart’s ability to pump blood and can cause life-threatening arrhythmias.
The goal is to identify the patients who might qualify for the program early in the process, so that they don’t arrive in the emergency room and CICU unexpectedly as they have in the past, said Powers. “We have a team that meets monthly and reviews the list of high-risk patients. We talk about what their risks are, what their anticipated needs are for labor, delivery and postpartum.”
Depending upon the needs, the team might include representatives from the CICU, Obstetrics (including a specialized pharmacist), Labor & Delivery, Cardiology, Advanced Heart Failure, Electrophysiology, Cardiac Anesthesia and Cardiac Surgery departments. “Everyone knows about the patient before they arrive. The patients are also seeing our cardiologists along with their regular OB visits,” Powers said.
“Collaboration will be one of the keys to attaining our mission, and it’s already taking place every day at Pauley,” he said.
The team creates a plan for each patient that is placed in their file, said Patterson. “We talk about special needs during their stay, maybe certain lines, medicines, or devices they will need—such as an intra-aortic balloon pump, pulmonary artery catheter or a Vigileo monitor.” She added, “Myopathies affect the muscle, which makes it weak. Some patients require LifeVest, an external defibrillator, that they wear during and after their pregnancy.” The patients check into the CICU the night before their scheduled C-section or induction and undergo any necessary testing or precautions.
Patterson recalls one patient in the high-risk program with a cardiomyopathy, who was also on a CPAP for 18 hours a day, who was at risk of having an emergency early delivery. She was admitted to the CICU very early in her pregnancy for a short stay to help optimize her situation. The team worked closely with the patient to prepare her for what to expect and sent her home with a LifeVest.
The high-risk patient was able to carry to full term and delivered a healthy baby. “She did fine and was discharged four days later,” recalled Powers with a smile. “She’s much more educated…and is engaged in follow-up care with specialists in Advanced Heart Failure.”
Multidisciplinary care is a key part of Hundley’s vision. Named Pauley’s first director in 2018, Hundley is a renowned leader in the field of cardiac MRI as Principal/Co-Investigator and Imaging Core Lab Director with a lifetime achievement of significant contributions on NIH-sponsored multicenter trials such as the WFSM Claude D. Pepper Older Americans Independence Center, Multi-Ethnic Study of Atherosclerosis (MESA), Preventing Anthracycline Cardiovascular Toxicity with Statins (PREVENT) and Understanding and Predicting Breast Cancer Events After Treatment (UPBEAT) to assess meaningful cardiovascular preventative, diagnostic and therapeutic end points in multiethnic, cardio-oncology and geriatric populations. His multidisciplinary approach and research expertise make him especially qualified to lead Pauley into its next chapter.
Since his appointment, he has led the first-ever research conference between the MCV and Monroe Park campuses. New faculty include those dually appointed between Pauley and other departments. In addition to taking part in research, they move between the two campuses, teaching a new generation of cardiac care providers.
Some of the dual appointees are Drs. Canada and Jordan, along with biomedical engineer Dr. John Wilson, whose research focuses on the biomechanics of aortic aneurysms and cancer-related cardiovascular toxicity; behavior and health policy scientist Dr. Alex Lucas, whose focus includes exercise interventions for cancer patients and survivors; and Dr. Salvatore Carbone, a nutritionist whose studies include an exploration of the effects of a Mediterranean-style diet on patients with obesity and a specific form of heart failure, called heart failure preserved ejection fraction (HFpEF).
Multidisciplinary teams, such as the cardiac sarcoidosis team that includes Jordan as well as Dr. Jordana Kron, Dr. Greg Hundley and Dr. Antonio Abbate, are zeroing in on important treatments for rare conditions (read online: Dr. Jordana Kron is searching for answers to a mystery disease).
Another team, Dr. Antonio Abbate and his colleague from Pharmacy, Dr. Benjamin Van Tassell, have worked together for 10 years developing and exploring the anti-inflammatory drug anakinra, an Interleukin-1 (IL-1) blocker, to treat heart failure. They began with preclinical studies, then small clinical trials. Their work has come to fruition: They are now busy enrolling patients in REDHART2, a phase II clinical trial to test anakinra on 102 patients, funded with a $2.7 million grant from the National Heart, Lung, and Blood Institute.
Both teams received their first funding in the form of pilot studies funded by Pauley donors, said Hundley. Donors also made the new Cardiovascular Imaging Lab and Hundley’s recruitment possible with $9 million in gifts.
“Our philanthropic supporters are providing the seed funding for innovative research, recruitment and improved facilities. They are helping us achieve our mission to be a premier site for the delivery of cardiovascular care, encompassing excellence in clinical care, education and research,” said Hundley.
Building on the new advances in technology in recent years, multidisciplinary teams that bring together people of different backgrounds and talents are helping to define Pauley’s newest chapter and fulfill its mission.
“I think Pauley will be a beacon to others for how to deliver cardiovascular care in the future.”
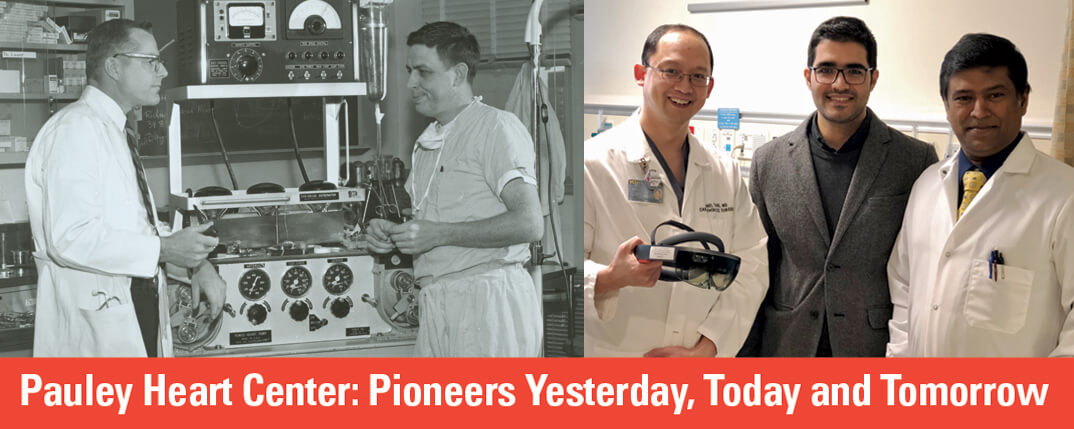
ABOVE: DR. RICHARD LOWER (LEFT) AND DR. RICHARD CLEVELAND, WITH ITS PREDECESSOR: THE PEMCO HEART PUMP. RIGHT: DR. DANIEL TANG; ALI PANAHI, COMPUTER SCIENCES GRADUATE STUDENT; AND DAYANJAN “SHANAKA” WIJESINGHE, PH.D., HAVE WORKED TOGETHER TO DEVELOP AR TECHNOLOGY FOR MEDICAL USE.
Back to Autumn-2019

